Jun 28, 2023
Transcript
MOLLY WEBSTER: Hey, it's Molly Webster. I am the senior correspondent here at Radiolab, but on this episode, I am a reporter bringing you two stories about things invading the human body. So buckle up, get ready. The first story is a story that we put out during COVID when we were doing something called Dispatches. Jad and I were kind of pumping out these weekly quick episodes about the pandemic, about what was happening with the virus, things that we were learning. But even though it's a COVID story, I think it's a really interesting one because it feels really universal in that it is a story about how when a virus gets into a human body, or really any body, the longer it's inside the body, the greater chance it has to mutate and to test out its offenses on the body's defenses. And so we're focusing on COVID, but the things that you hear in the story are things that can happen in HIV, with the flu, with other coronaviruses. So listen with ears wide open, because it feels like a pretty universal story that was told at a very specific time.
[RADIOLAB INTRO]
JAD ABUMRAD: Webster, are you there?
MOLLY: Yeah. That was amazing. You started coming—I still don't see you.
JAD: I'm Jad Abumrad. This is Radiolab. I just wanted to play you a conversation I had with senior correspondent Molly Webster. She and I check in every Friday morning, where she usually just kind of updates me on new research she's following things she's been interested in. And she told me about a few new studies that she had just read. These are articles about different individual COVID patients from different spots around the world, and each paper looked at how the virus behaves inside a single human body. One, a case study from the UK, starts with a man in his 70s coming into a hospital with an immune system that was already pretty low.
MOLLY: Yeah, his immune system was low because he had lymphoma.
JAD: Uh-huh.
MOLLY: And then was on a drug to try and keep the cancer in check. And that lowers your ...
JAD: Got it.
MOLLY: ... your immune system.
JAD: So this man in his 70s ...
MOLLY: He had a suppressed immune system, and he shows up in a hospital because of cancer stuff. And while he's there, they test him and he's positive for SARS-CoV-2.
JAD: Okay.
MOLLY: But he seems relatively fine, and he just has, like, a small cough or something. And so they send him home. And then 35 or 34 days later, on day 35, he walks back into the hospital, and what had been a cough for the last month had, like, turned into shortness of breath.
JAD: Huh.
MOLLY: And they test him again, and he has coronavirus.
JAD: Which most likely meant that he had coronavirus for the whole month and couldn't get rid of it.
MOLLY: So he tests positive for coronavirus, and he has, like, the COVID-19 pneumonia, kind of that settles into your lungs.
JAD: The crackly cough thing?
MOLLY: Yeah. You know, the gray spots on the lungs that they, like, identify in CT scans and stuff?
JAD: Yeah.
MOLLY: And so they check him into the hospital, and then what basically starts is just a series of trying to treat this man. At the same time, the UK is actually really good about taking samples and genetically sequencing them, as we all know, in a way that America is not doing right now. And so over the course of his time in the hospital—and he does eventually end up dying on what they say is day 102.
JAD: Oh, wow!
MOLLY: Over the course of that time, they sequence his virus 23 times.
JAD: So basically, over the last three-and-a-half months of this man's life, the doctors take snapshots of the virus inside him. You can think of these as a series of stills that capture what the virus is doing, how it is moving. You can think of them as mugshots, a series of mugshots. Now at this point, going back a year, there was really only one main version of SARS-CoV-2 that was out there, or at least in our consciousness. There weren't all of these variants from South Africa or Brazil.
MOLLY: Or the New York City variant.
JAD: There's a new one?
MOLLY: Yeah.
JAD: I did not ...
MOLLY: The New York City one is new, and now there's a new Oregon variant.
JAD: Oh, snap!
JAD: None of that was on our radar. Yeah, we were just focused on the original.
MOLLY: The original. Like, what I call, like, OG SARS-CoV-2.
JAD: That was the perp that the doctors expected to see on all those mug shots. And they did see it on day one, but then when he went away and came back 34-ish days later and proceeded to get sicker and sicker in the hospital, they sequenced again, and this time they saw something different. Instead of just one COVID virus inside him ...
MOLLY: They saw pop up, like, little subpopulations.
JAD: They saw a whole bunch of different kinds.
MOLLY: With enough variation that they look different.
JAD: Huh!
MOLLY: What they noticed is, like, oh, there's still the dominant, like, OG SARS-CoV-2 genetic sequence all over this body.
JAD: Okay.
MOLLY: But there's really small, quiet, like, subpopulations that are hanging around. And at the time, they were like, "Whoa, whoa, whoa. There's all these, like, variations! Well, has this person been infected by, like, six different types of this virus, and they all happened to get into this person at the same time?"
JAD: Oh, like, he somehow managed to have six different encounters with six different coronaviruses?
MOLLY: Or, like, day one, he had a case, and then it cleared.
JAD: Yeah.
MOLLY: And then maybe got it again.
JAD: And then again and again and again. So the doctors at that point have a new thought: maybe this isn't the same infection that he's had the whole time. Maybe these are separate viruses, entirely separate.
MOLLY: But then they realized no, this is one strain that got in and just keeps changing, changing, changing, changing, changing.
JAD: In other words, what the researchers came to understand—and they weren't trying to study this, they were simply trying to save the man's life, is that these subpopulations were one virus rapidly mutating, trying out new forms inside a human body. That when you have a human body that has a compromised immune system, the COVID virus will just rapidly experiment.
MOLLY: That the immune-suppressed body is like a playground of sorts because, like, nothing actually shuts the virus down, and it can replicate uninhibited. This one researcher said that at any point in time when you're, like, infected with coronavirus, you can have, like, at least a billion copies of the virus inside of you.
JAD: One billion?
MOLLY: One billion.
JAD: Oh my God!
MOLLY: And so that means that every time it replicates, it has a chance to, like, mutate, substitute, delete one little nucleotide.
JAD: But I thought the whole deal with the coronavirus—I mean, you and I did a story about this—is that unlike the other RNA viruses, which are super sloppy, the coronavirus actually catches its own mistakes pretty well and doesn't mutate that much.
MOLLY: So it doesn't actually mutate that fast, but it still does just mutate. And every time it replicates, there is a chance that a mutation can set in and hence evolution can happen, right? Because if you change part of your genetic code, you have a chance to, like, have new characteristics that let you survive in the world in a different way.
JAD: Hmm.
MOLLY: And so if it's in the body and it's allowed to replicate a billion times with really nothing to stop it, every time it replicates, you throw the dice and something can happen.
JAD: So getting back to this guy, the researchers noticed that he's got all of these different subpopulations of SARS-CoV-2 viruses, different kinds inside of him. But most of the new variants?
MOLLY: They're not really doing much. They don't have much dominance. Like, if you actually look at the numbers, I think it's something like—I may be making this up but I don't think I am, but it's something like the original genetic virus is almost at 100 percent dominance, and every other little subpopulation is, like, less than two percent.
JAD: But then, she says, the doctors start to give this guy treatments.
MOLLY: So he gets to hospital, day 35. Day 41, they do a round of remdesivir.
JAD: That's one of the few drug treatments available against the virus.
MOLLY: Day 54, they do another round of remdesivir. And then on day 63, they give him convalescent plasma from a donor. And this is like the blood you take from the body of a person who has successfully fought off CoV-2, and you put it in a person who's struggling to mount an antibody defense system to, like, take the virus down.
JAD: The thought is—and this is also a story we've done—the antibodies in the survivor's blood will help you fight off the virus. So day 63, guy gets infusion of plasma.
MOLLY: And then on day 65, they give him another batch of convalescent plasma. So they're, like, giving treatments, and then as they're giving treatments, they're taking samples and genetically sequencing them. And what they see is that by the time they check his samples in, like, the 80s, like day 82 or day 81, the different subtypes have, like, exploded.
JAD: Really?
MOLLY: And there are, like, very noticeable changes in the coronavirus inside his body.
JAD: More on that after the break.
JAD: This is Radiolab. I'm Jad Abumarad. Today we are in Molly Webster territory. Actually, we are in the middle of a recording of her and I's weekly meeting where she was telling me about some papers that have just come out that show how the SARS-Co-V2 virus behaves inside a single human body. I also just want to say before we rejoin that conversation, God bless the man in the UK, the human beings who are at the center of these case studies. Papers kept their identities secret, of course. We will obviously do the same.
JAD: But in a few of these cases—not all—these people passed away, and they allowed doctors to study them in the final months of their life so that we could all learn something about the nature of this enemy. So endless gratitude to those people. Okay, so before the break, Molly was explaining that in this man in the UK with the compromised immune system, the doctors first noticed that there were all of these variants of the coronavirus popping up, like, all these different subpopulations. Which were basically kept in check for a while, but then as soon as the doctors started trying to treat the patient with drugs and convalescent plasma, those subpopulations just explode.
MOLLY: And there are, like, very noticeable changes in the coronavirus inside his body. They see, like, these deletions that they call, you know, deletions at 69 and 70. And then there's this other mutation, it's something called 796. It's very wonky, like, all based on amino acid positioning.
JAD: Okay.
MOLLY: And suddenly, that virus variant is, like, dominant.
JAD: Huh!
MOLLY: And the OG SARS-CoV-2 virus variant has become a quiet subpopulation.
JAD: Weird! So okay, help me unpack what that ...
MOLLY: Yeah.
JAD: I don't quite know how to hear that. Does that mean that whatever it was in the plasma, whatever antibody army came in from the donor, obliterated OG SARS, but it somehow allowed for this little subpopulation to just bloom?
MOLLY: Essentially. So what they say is like, "Oh, my gosh. We added in all of these antibodies, and we've just witnessed how SARS-CoV-2 might try and get around those antibodies.
JAD: So they basically witnessed evolution happening right in front of them.
MOLLY: Yes.
JAD: Is that the way to say it?
MOLLY: That is right.
JAD: And in the example you just gave, where there was a mutation in 69 or 70 or whatever it was, what does that actually do for the virus?
MOLLY: So the 69, 70 deletion on its own makes the virus twice as efficient at infecting cells.
JAD: Really?
MOLLY: And they think that's because it can clamp on more tightly to your cells. And so if you have that variation, you bind more tightly, which means, like, when you inject your genetic material, it all gets inside, and, like, the cell can't shake you.
JAD: Okay, so we're only at stage one here. So they see this scary mutation bloom in this one patient, this poor man. And then Molly says as they kept trying to treat the man and then test him to measure the effect of those treatments, they saw this kind of real-time evolution just continue and escalate. They'd see all of these different populations come and go, rise, fall.
MOLLY: There might be two different types, and they rise and fall together. And then there's some where, like, if virus variant A is in there, D won't survive. I have this, like, little part of the paper cut out. I'm just gonna read it to you.
JAD: Yeah.
MOLLY: It says, "Patterns in the variant frequencies suggest competition between virus populations carrying different mutations. Viruses with the mutation deletion pair spike letters 796, 6970 rose to high frequency during convalescent plasma therapy, but were then outcompeted by another population in the absence of therapy. Specifically, these data are consistent with a lineage of viruses with the NSP-2-I-513T, and RDP—no, RDRP-V-157-L variant, which was dominant on day 66, but was outcompeted during therapy by the mutation deletion variant." That's 796 and 6970. "With the lapse in therapy, the original strain, which had acquired NSP-15-N1773-S N spike Y-200-HT-240-I regained dominance, followed by the emergence of a separate population with the [00:15:00.09]spike W-64-GP-330-S variant." [laughs] Oof! That's like, one paragraph from the paper.
JAD: So those are all different, like, subpopulations of coronaviruses that are kind of duking it out in this one guy? Wow!
MOLLY: In that one patient in the UK. This is just from that paper.
JAD: Dang! How many different corona tribes are we talking about?
MOLLY: So there's 501-Y, 796, 6970, 240-I, 200-H, 330-F, W-64-G, I-5-13-T, V-157-L, N-1773-F. So something like at least 10 different populations rose and fell.
JAD: Whoa!
MOLLY: Some of them exist all over globally, some exist in different parts of the body. And they're all having different types of battles with the things that you're putting inside, and then they're all having different types of battles with each other.
JAD: And they're seeing this in a single human?
MOLLY: Yes, a single person.
JAD: Wow! I don't know why, but this is completely blowing my mind!
MOLLY: Well, because one of the scientists described it as like, you can see a single body, a single patient as, like, a battleground or a training ground.
JAD: Oh, wow! That's scary!
MOLLY: [laughs] Yeah, I know! If you can look in and follow the action, it's almost like The Truman Show, but rather than us being in The Truman Show, you're looking in—you're looking into The Truman Show, like, watching the world change and be manipulated, and you're like, "Now I want to make it rain."
JAD: Whoa!
MOLLY: "Now I will cause a tornado, and I'm gonna see, like, how the world react—how this world reacts to that." It's just like a whole microcosm inside one person.
JAD: And in that passage you read, it said that the different populations of coronavirus are competing. Are they fighting? How are they fighting?
MOLLY: It's not fighting. It's all about real estate, really. It's like, can you get in a cell? How fast can you get in a cell, and how quickly can you replicate in that cell? If you think about the body, there is a limited number of cells for the virus to infect, and so if it wants to make lots of different types of itself—and I'm saying 'wants' like it has, like, a wish. If it wants to make different types of itself, all of those different variants are fighting for the same real estate.
JAD: Huh!
MOLLY: Like, there's one paper about a patient who had coronavirus—who was immune suppressed, had coronavirus for at least 70 days. Asymptomatic. Eventually, it cleared their system, but they saw the virus, like, mutating inside this one person. There's something that medicine can witness. I think it's not even, like, learn, it's actually like, what we can witness is, in a sense, everything that is happening out in the wild but, like, in one place, which happens to be ...
JAD: Whoa, whoa, whoa.
MOLLY: Oh, yeah. I just did a big jump, yeah.
JAD: You just made a jump, which was where my mind was going, which was—okay, so if we zoom out just a bit and we look at this one body, and we see that these variations, these different populations that are rising and falling and competing for real estate, is there anything that they are seeing in these single human cases, inside of these single immunosuppressed people, that is mirroring what we're seeing out in the world in terms of all the different variants that are floating around in South Africa and Brazil and all that?
MOLLY: So that's where it gets really spinny. That's where it gets really trippy, is that these patients end up being like a blueprint. Like, with them, you could see what the virus might do in the future. And to break that down, what they saw happen inside those bodies were the formation and creation of mutations that then appeared out in the wild six months later in, like, the UK variant, the South African variant, and the Brazil variant that we're all, like, running scared from.
JAD: Whoa!
MOLLY: Five months before a scary virus variant showed up in the wild, they saw it inside a person.
JAD: Okay, okay, okay. If they're seeing these mutations dominate in immunocompromised bodies before they dominate in the wild, does that tell them that they started in the immunocompromised bodies and then got out into the wild?
MOLLY: Well, so that's an interesting question. So with these specific case studies that were written up, whatever happened inside the body never left the body because the patient was in hospital the whole time and closed down.
JAD: Oh, okay.
MOLLY: But the thought now is, based on two of these case studies and a few others that have come out, is that probably, at least the UK variant, that B-117, came out of an immunocompromised body, because they said that variant has, like, eight significant mutations in it, and in order to get that in the wild, it would take many, many months. And if you were genetically sequencing, like they do very frequently in the UK, you would see the tracings of that change start to happen.
JAD: Oh, interesting!
MOLLY: You'd be like, "Oh, there's a change here." That's change one. "There's a change here." That's change two. "There's a change here." That's change three. But everyone said one day they woke up and there was a new virus with, like, eight significant changes, which makes them think that, like, that all happened in one hidden place and then, like, burst onto the scene.
JAD: That's so funny, because that was the experience of consuming the news was that like, "Oh, you know, Co-V-2." And then, like, I remember hearing that, like, it doesn't mutate that much. Okay, great. Whew! Glad to hear that. And we've got these vaccines coming in. Yay! And then suddenly, like, literally on a Tuesday, everyone's like, oh, snap, there's a variant. We've got a new variant. And I'm like, wait, what? Where did that come from?
MOLLY: Where did that come from? Well, scientists had the same reaction, and what they're saying is in these, like, immune suppressed patients, where you can witness the virus trying to adapt, and where you can, like, step by step see how it interacts with each treatment you give it, you can actually have a clue to, like, how the virus might change in the future. Because if ...
JAD: That's bananas! That's so weird. It's like seeing the future.
MOLLY: It is. It is. Like, this one guy called it a crystal ball. Another guy called it the harbinger of, like, what's to come in the virus.
JAD: That's so wild!
MOLLY: Yeah. The idea is, at some level, the virus can change a lot of ways, but at another level, it can only change so many ways. And so if you watch it mutate, like a million, two million, three million, four million, five million times inside a person's body, and you see which variants dominate, there's a pretty good chance that, like, okay, if the virus ever rolled the dice out in the wild and it landed on this mutation, this mutation would take hold and thrive.
JAD: So it's very possible it's gonna hit the same mutations in different places independently, and we might be able to see that in advance inside one person?
MOLLY: Yes.
JAD: Yeah. You know what I'm struck by?
MOLLY: Yeah?
JAD: It's really—it's interesting to hear this story right now, you know? Because it's like, from one moment to the next, it's really hard to know whether to feel optimistic or pessimistic, right?
MOLLY: Right.
JAD: You know, it's like—and kind of the story you're telling—and it's weird to, like, look outside and see, like, "Oh, it's sunny. Like, spring is coming. Like, the vaccines are rolling out. We might actually get to go have dinner with friends again." And everybody's like, in this kind of, like, "Ah, normal life is returning!" The story you're telling me is, like, is it? The virus is crafty, but then maybe so are we? I don't know. It's weird to juxtapose what you're saying against that sense of optimism that's out in the world, because what I'm hearing is that simultaneously, this virus is figuring us out, and we're figuring it out.
MOLLY: Yeah.
JAD: And maybe we're turning the corner, or maybe we're just in the first chapter of a very long story, you know?
MOLLY: Yeah. Like, I think I keep having a—having a lot of visuals. Like myself, and I would say my community are probably at the lowest ebb I've seen them at in the last year, but also with—with a whole bunch of, like, hope just starting to, like, glimmer. I keep thinking of that Midnight in the Garden of Good and Evil statue. Do you know what that is? It's like the little girl, and she has her hands up by her shoulders with her palms, like, up to the sky, and it's like good and evil are, like, weighted on each side. I feel like that feels like this moment in COVID to me where you're holding, like, optimism and pessimism. You're holding, like, hope and just, like, utter exhaustion on both shoulders.
JAD: Yeah. Wow. Yeah, that's exactly it.
JAD: Senior correspondent Molly Webster.
MOLLY: This episode would not be possible without the counsel and interviews with Ravi Gupta and Jonathan Lee. Thank you both so, so much.
JAD: Hey, I'm Jad Abumrad. This is Radiolab. And today, a story from our very own Molly Webster.
MOLLY: So yeah, so today we're talking about a medical mystery.
JAD: A medical mystery?
MOLLY: Yeah. It starts with a woman ...
JOVERIA FAROOQI: Hello?
MOLLY: Hi, I'm trying to reach Joveria, please.
MOLLY: ... named Joveria Farooqi.
JOVERIA FAROOQI: This is Joveria. How are you, Molly?
MOLLY: She works at a hospital ...
JOVERIA FAROOQI: At a teaching hospital in Pakistan.
MOLLY: ... in Karachi.
JOVERIA FAROOQI: the Aga Khan University. And I'm a medical doctor specialized in medical microbiology.
MOLLY: Joveria works in the hospital lab, and so when someone has an infection, she gets sent, you know, some blood or urine or something, and she tries to figure out which bug is causing the problem.
JOVERIA FAROOQI: So the very first month that I was in the lab ...
MOLLY: In the fall of 2014.
JOVERIA FAROOQI: ... the third week of October, I found three bugs.
MOLLY: In the blood of three different patients.
JOVERIA FAROOQI: Which looked exactly the same.
MOLLY: And like nothing she'd ever seen before.
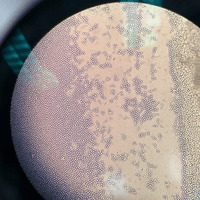
JOVERIA FAROOQI: Creamy in texture. It had a whitish rim, and had another ring of light brown around it. White center, and very, very white. It's sort of like when you put UV light on white and it sort of shines with a bluish tint.
MOLLY: And what she saw wasn't a bacteria or a virus. It was actually a fungus.
JOVERIA FAROOQI: A yeast.
MOLLY: But beyond that, she sort of had no idea what it was.
JOVERIA FAROOQI: I shared it with all my friends who were working in other labs, and I asked them if they had encountered something like this, and they all said no. But the patients were all very, very sick.
FAISAL MAHMOUD: Yeah, well, so what happened is that we started seeing patients with fever, high white cell count.
MOLLY: So the three patients those samples had come from were all at the same hospital, under the care of this guy.
FAISAL MAHMOUD: Dr. Faisal Mahmoud. I'm an infectious disease specialist here at the Aga Khan University.
MOLLY: And all three of them were patients in the ICU.
FAISAL MAHMOUD: Older patients, folks who've been in the hospital for a week or two weeks.
MOLLY: You know, with patients like that, they definitely deal with fungal infections from time to time.
FAISAL MAHMOUD: So the symptoms were really nothing spectacular, nothing weird.
MOLLY: But when he found out that they all came down with the same mysterious fungus all at the same time ...
FAISAL MAHMOUD: When it was identified, we're like, "Okay, that's weird."
MOLLY: Maybe some kind of coincidence?
FAISAL MAHMOUD: But then ...
JOVERIA FAROOQI: While I was looking at those, I encountered yet another one.
FAISAL MAHMOUD: Another one popped up.
JOVERIA FAROOQI: Exactly the same yeast.
FAISAL MAHMOUD: And another one popped up.
MOLLY: In the same hospital, but this time not from the ICU.
JOVERIA FAROOQI: And I thought, oh, my God!
MOLLY: Which was really strange, because they had never seen this fungus before, and suddenly it's popping up all over the hospital.
JOVERIA FAROOQI: I would have been okay if it was just one case or two cases in a whole year. That's all right. However, to encounter them in a cluster is alarming. You know, what's it doing in our hospital, behaving so angrily and killing people off? I mean, two of our patients had died by then.
FAISAL MAHMOUD: You know, we just sort of kept seeing them. Tuck, tuck, tuck, tuck. I think within six months, we had, like, 19 cases.
MOLLY: And by then, six months in, eight of the patients had died.
JAD: So this fungus is pretty nasty.
MOLLY: Yeah. I mean, the people who get it seem to have other sicknesses as well, but once you got it, the mortality rate's, like 20 to 60 percent.
JAD: Oh, damn!
FAISAL MAHMOUD: And that's about the same time when Joveria sent some strains to the US CDC.
MOLLY: Joveria basically sent them an email and just said, you know, "Hey, will you look at this thing?" And this is when the mystery of this fungus went way, way beyond one hospital in Pakistan.
TOM CHILLER: We were informed by colleagues in Pakistan that they were having a large outbreak.
MOLLY: One of the guys that got that email eventually was Tom Chiller.
TOM CHILLER: Chief of the mycotic diseases branch here at the Centers for Disease Control and Prevention in Atlanta, Georgia.
MOLLY: And he and his colleagues pretty quickly identified the fungus as ...
TOM CHILLER: Candida auris.
FAISAL MAHMOUD: They said, it was candida auris. And I'm like, "Candida what?" I was like, "I've never heard of candida auris before."
MOLLY: Now candida is kind of a big group of fungus. It lives on our skin and in our gut, and can cause yeast infections and thrush in babies. But this particular candida was totally new.
TOM CHILLER: It was first isolated from an ear infection of a Japanese patient.
MOLLY: And that was in 2009. And it was really just causing some sort of goopy goop to leak out of this woman's ear.
TOM CHILLER: On the skin where we know some candida species can be. And we didn't think, honestly, much of it.
MOLLY: Until six years later, they hear from Joveria that this candida auris is getting into people's blood and causing serious infections.
TOM CHILLER: You know, horrible bloodstream infections and even death.
MOLLY: And so he thought, okay, this thing that we saw once that we did not think was a big deal is now killing people. So what's going on? And so he started poking around, and he came across reports of candida auris outbreaks in South Korea, in India.
TOM CHILLER: And South Africa had described clusters.
FAISAL MAHMOUD: And we figured we found out that it's popping up all over the world.
MOLLY: And actually, while looking into this ...
TOM CHILLER: Colleagues from London were talking to us about a very similar phenomenon with the same organism.
MOLLY: A hospital in London had an outbreak.
TOM CHILLER: To the point where they had to close their intensive care unit for a period of months. So what we saw were that there were essentially four different clades, for lack of a better word, that were emerging in three different continents, all about at the same time.
MOLLY: Meaning it wasn't like it started in one place and then went to all these other places.
TOM CHILLER: It couldn't be explained by travel, it couldn't be explained by—you know, by the fact that these were in some way related, except that they were the same species of organism. They truly were emerging at around the same time in four parts of the world.
MOLLY: So the big question that arises out of this moment is: why now?
TOM CHILLER: Yeah.
JAD: Wait, just so I make sure I'm getting this, you have one fungus appearing in four totally different parts of the world, simultaneously?
MOLLY: Simultaneously.
JAD: Weird!
MOLLY: It's definitely not normal.
SNIGDHA VALLABHANENI: No, it's absolutely abnormal. And, you know, people around the world are trying to figure out how this happened, why it happened. Why is it ...
MOLLY: So this is Snigdha Vallabhaneni, and she was part of the team at the CDC that was tracking the fungus and trying to figure out what was going on.
SNIGDHA VALLABHANENI: So initially, we thought, like, could—is it possible it's some contaminated medical product, or something that got distributed?
MOLLY: Something that got distributed to these hospitals. But then they thought, four different hospitals on three different continents?
SNIGDHA VALLABHANENI: I mean, you don't expect it to be that worldwide.
MOLLY: So it's like, scratch that. Maybe it's ...
SNIGDHA VALLABHANENI: The way, you know, different antifungal drugs have been used around the world.
MOLLY: Like, we all use, you know, antifungals in our body, but the more important thing is farms using antifungals, where they spray their crops. So it's maybe the fungus are adapting to fungicides and it's just getting stronger.
JAD: So would it be that the farmers are treating the fungus, and then those fungus are then somehow getting away from the farm and into the hospitals?
MOLLY: Yeah.
JAD: Okay.
MOLLY: But that still doesn't explain why it would happen in all these separate places at this one particular moment.
JAD: Why now?
MOLLY: Right. You need something that was happening to all of these fungus in different places at the same time.
SNIGDHA VALLABHANENI: That's why people are looking for more of this, not just environment, but sort of a bigger picture, ecological analyses.
JAD: Meaning what?
MOLLY: Well, I just at this point, feel like I should just start talking about dinosaurs.
JAD: [laughs] Wait, wait, wait.
MOLLY: It is a little bit of a detour, but I promise it will pay off.
JAD: No, it's my relationship with dinosaurs in general. So I'm like, "Oh, God, here we go!
MOLLY: There's a lot of history there.
[ARCHIVE CLIP, announcer: Ladies and gentlemen, please welcome to the stage your hosts for this evening, Jab Abumrad and Robert Krulwich!
[cheers]
MOLLY: But trust me, it'll be worth it.
[ARCHIVE CLIP, Jad Abumrad: What's up, Seattle?]
JAD: To loop everybody in, about seven years ago, we did a live show called Apocalyptical that had life-sized dinosaur puppets, traveled 21 cities. Super fun, but it completely broke us, and we all nearly died.
MOLLY: [laughs] Yeah, it's true. But part of that live show is a story that I reported for you guys about an asteroid that hit the earth and put an end to the dinos.
[ARCHIVE CLIP, Jad Abumrad: So it turns out on that day, as the fire was raging above on the surface, somewhere in a little hole in the ground, happened to be a furry little animal.]
MOLLY: And about how, after the cataclysm, this mammal, small little mammal, crawled out of its little muddy burrow into a dinoless world and became the ...
[ARCHIVE CLIP, Jad Abumrad: Great great great great great, et cetera, grandma of everybody in this room. It is true. There was a creature down there. There was a creature down there ...]
[ARCHIVE CLIP, Robert Krulwich: I thought we should stop there because we were getting away with something, and I didn't want to push it too far.]
[ARCHIVE CLIP, Jad Abumrad: All of a sudden, it was just you and me.]
[ARCHIVE CLIP, Robert Krulwich: Yeah.]
JAD: Aww! I miss Robert.
MOLLY: I know.
JAD: [sighs] Anyhow, continue.
MOLLY: The story goes like this: with dinosaurs out of the way, the idea is that mammals crawled out of the hole and they just inherited the Earth. So big reptiles out, crafty little mammals in.
JAD: Yep.
MOLLY: But there is a new idea about this fungal friend of ours, this one we've been talking about, that sort of messes this story up a little bit.
ARTURO CASADEVALL: So here we are in the realm of hypothesis, speculation. We don't really know what happens 65 million years ago or 100 million years ago.
MOLLY: The idea comes from this doctor and microbiologist, Arturo Casadevall at Johns Hopkins University. And he says the first few beats of our story are all good.
ARTURO CASADEVALL: Right. We know that there was a catastrophe. the asteroid hit the Yucatan, and we know that the earth had a really bad day, and the animals that then follow are—Is the age of mammals.
MOLLY: Yeah. Because I feel like we, like, took down all those dinosaurs and there was a big hole and we're like, "Ah!" And we crawled out of it.
ARTURO CASADEVALL: Yeah. I think that people thought that, you know, because the dinosaurs were wiped out, that it created a space.
MOLLY: This is absolutely what I think.
ARTURO CASADEVALL: Right. So there is a little bit of a problem with—in my mind with that, and I add that this is my problem. [laughs] But I'll show you what the thinking is. If you look at our world today, we still have reptiles.
[ARCHIVE CLIP: A crocodile-infested riverbank.]
ARTURO CASADEVALL: We have alligators.
[ARCHIVE CLIP: This is a gaboon viper from West Africa.]
ARTURO CASADEVALL: We have lizards.
[ARCHIVE CLIP: A monitor lizard is out hunting, looking for the entrance to the galleries in which the mammals take shelter during the daylight hours.]
ARTURO CASADEVALL: So clearly, some reptiles survived the catastrophe.
MOLLY: There were reptilian creatures that were living in the, you know, riverbank in the same way that the mammals were, and got out of the fires and the ash and came out.
ARTURO CASADEVALL: And it's always bothered me how come we didn't have a second reptilian age.
MOLLY: So you actually have a moment when either of them could have taken the crown.
JAD: I thought the idea was just we got lucky.
MOLLY: I mean, we would have had to be really lucky, because according to Arturo, reptiles had two big advantages over us straight out the gates. First one being ...
ARTURO CASADEVALL: Reptiles, in contrast to mammals, don't need that much food.
MOLLY: Which, you know, is great, because at the time, most of the plants had burned up, the planet was covered in ash, there really wasn't that much food. And whereas mammals have to eat all the time, like, reptiles can just chill for a while. So that's definitely a win for reptiles over mammals.
ARTURO CASADEVALL: They also reproduce a lot faster.
MOLLY: The second one is that they just make more babies. They can spread a lot faster. Their chances of survival are greater. So Arturo's like ...
ARTURO CASADEVALL: If the reptiles are able to do well with less food, and they reproduce faster, why didn't they just take off and create a whole new world which is reptilian, too?
MOLLY: Now his idea for why this didn't happen, why there wasn't a second reptilian age, is that there is another player on the dino-free stage.
JAD: Hmm.
MOLLY: A small, invisible, yet powerful player. And to understand, you have to know that before the asteroid hit ...
ARTURO CASADEVALL: It was a forested planet that was, in fact, a lot warmer than it is today. There were forests in many parts of the world. The cataclysm is thought to have led to rapid temperatures that fell. And you also had no sun. So imagine a dark, cold world of decaying vegetation. This cataclysm was associated with a massive proliferation of fungi.
JAD: Huh!
MOLLY: And actually, if you look at, like, right above the KT Boundary, that line that demarcs, you know, no meteor/meteor, no dinosaur/dinosaur.
JAD: Yeah.
MOLLY: If you look right above there, the soil is filled with spores.
JAD: No [bleep]!
MOLLY: And so everyone knows, it's really well documented that ...
JAD: Wait, so as a layer after the impact ...
MOLLY: Yes.
JAD: There is a layer one or two up which is filled with fungi spores?
MOLLY: Yes.
JAD: That's interesting.
MOLLY: And so he said it's very well known that there was fungus growing on things that got burned. Fungus probably just growing cause it's wet and damp, and why not?
JAD: So there's mold and mushrooms everywhere.
MOLLY: There's also dead bodies. There's, like, things decomposing.
JAD: Which fungus likes.
MOLLY: They love, I've heard at parties.
JAD: [laughs] So it looks like you have a couple of shrew-like creatures walking around. You've got some alligators, but you've got a crapload of fungus.
MOLLY: And you got a crapload of fungus.
ARTURO CASADEVALL: Fungus.
MOLLY: Is it fungi? Fungi? Fungi. Is he a fungi or is he the fungi? Probably fungi.
ARTURO CASADEVALL: I would say whatever you like.
MOLLY: No, probably whatever you tell me.
ARTURO CASADEVALL: No, seriously. Some people pronounce a fungi. Some people pronounce fungi.
MOLLY: Okay.
ARTURO CASADEVALL: Or fungi. [laughs]
MOLLY: Anyways, whatever you call it, if you are an animal, a reptile, or a mammal, fungi can be deadly.
ARTURO CASADEVALL: That's right.
MOLLY: And while reptiles could skip meals and make a bunch of babies, when it came to fending off fungi, we had an advantage.
ARTURO CASADEVALL: We have two pillars that protect us. One of them is that we have advanced immunity.
MOLLY: The immune system is obviously like the kung-fu fighter. It really takes up the weight of keeping something out.
ARTURO CASADEVALL: But the other thing that we have that frogs don't have, and that trees don't have, and that insects don't have is that we are really hot relative to the environment. We are warm. We are warm blooded.
MOLLY: Mammals actually use some of their energy to keep their bodies warm. So if you think about us, it could be really cold outside, it could be really hot outside, but we stay at a steady, basically 98.6. Now if you're fungi, you actually like it kind of cold.
ARTURO CASADEVALL: They do very well until about 30 degrees.
MOLLY: Like 86 degrees Fahrenheit.
ARTURO CASADEVALL: Right.
MOLLY: Any hotter than that ...
ARTURO CASADEVALL: It denatures them irreversibly.
MOLLY: Their proteins start to fall apart, their cells start to melt. And so if a post-apocalyptic fungi got into a post-apocalyptic, very warm mammal, it would die.
ARTURO CASADEVALL: These high temperatures creates, you know, a heat barrier. And this heat barrier means that the majority of fungal species out there cannot grow or replicate inside your body because you're too warm.
MOLLY: Our heat keeps the fungus out.
ARTURO CASADEVALL: You got it.
MOLLY: If you are a reptile, you're cold blooded. You don't have a way to keep yourself, like, steady and warm. You have to go look for ways to become warm. You know, have you ever seen lizards lie on rocks? You know where they're just, like, out in the sun, soaking up the heat?
JAD: Sure.
MOLLY: So that will warm their bodies up, but also—and I never knew this, it also will clear, like, fungus from their body.
JAD: Oh!
MOLLY: So if they're sick, because it warms them up so much, that warmth attacks the fungus.
JAD: Do they not do fevers?
MOLLY: They can't do fevers. So their way of getting as hot as possible is doing that sunscape thing.
JAD: [bleep]
MOLLY: I know! So he was saying that if you're a reptile and you get a fungus but there's no sun to warm yourself in because—because the apocalypse has just happened ...
JAD: It kicked up the dust, blocked out the sun. Nuclear winter.
MOLLY: Mm-hmm. So you die because you can't withhold the fungus. But if you're a mammal, the fungus comes, your body temperature naturally kills it. And so suddenly, his theory goes ...
JAD: Interesting!
MOLLY: ... you have mammals filling the hole and really flourishing in a way they never did before, because fungus helped them do the mammalian explosion.
ARTURO CASADEVALL: Right. Because we went through this fungal filter, and therefore we are now a fungal filter at the end of the Cretaceous.
JAD: Wow!
MOLLY: Now it gets even weirder, because then Arturo decided he wanted to find out if you are warm blooded ...
ARTURO CASADEVALL: What was the optimal temperature by which you get the most protection against the fungi, and yet you don't have to eat all the time?
MOLLY: What is the optimal temperature to keep us from eating all the time but still give us defense? The reason we eat three meals a day is to stay warm and functioning. If we were less warm, we could eat less.
JAD: Oh, so it's like, how little can we eat and still be protected against fungus and ...
MOLLY: Yes.
JAD: ... stuff.
ARTURO CASADEVALL: That's correct. And what Aviv did ...
MOLLY: And so what Arturo did was he got together with this mathematical biologist, Aviv Bergman. And first, they just gathered some numbers.
ARTURO CASADEVALL: What is the temperature susceptibility of fungi?
MOLLY: Like most fungi don't like it above 86 degrees Fahrenheit.
ARTURO CASADEVALL: And then he looked at the well-known formulas for calorie use, and then he asked the question: if you put these two formulas together, what is the best temperature that keeps out most fungi, but doesn't require you to have to eat all the time?
MOLLY: They basically crunched a number that had to do with, like, how many calories you need a day, and just like, the energy that would take of eating and then keeping out pathogens.
ARTURO CASADEVALL: And what he found was that our temperature ...
MOLLY: 98.6 degrees.
ARTURO CASADEVALL: ... is that temperature that best balances protection against the fungi versus the need to eat food.
JAD: Whoa!
MOLLY: Bing, bing, bing!
ARTURO CASADEVALL: We were amazed and tickled by it.
JAD: He's saying the reason our bodies are precisely 98.6 degrees is because of fungus? Like, they shaped us to be that?
MOLLY: My heart wants to say yes. But to caveat, he did say it could be totally correlational.
ARTURO CASADEVALL: Right.
MOLLY: Obviously, he's not been able to take the temperature of any of our ancient ancestors. But, you know, it is a very interesting idea that part of being a mammal is about being good at fending off fungi—unless part of that equation changes. So this brings us—some might say finally—back to our medical mystery, which is that Arturo wonders what if, in light of this dino-mammal-fungus detente, this thing that seems new, candida auris, has actually been here the whole time. So say these fungi typically live outdoors in soil and on rocks. And they live in a place that's like, you know, normally 75 degrees.
JAD: Hawaii.
MOLLY: You want—okay.
JAD: Let's say Hawaii, because they're big into mushrooms there.
MOLLY: Their ideal temperature is 77 degrees. And if they go above that, they start to feel a little queasy, really start to fade, and it's a struggle.
JAD: Right.
MOLLY: Okay, so one day it's 81 degrees, and, like, the fungus are like, "Oh, [bleep] this is hot!"
ARTURO CASADEVALL: All fungi have the capacity to tolerate short burst of heat, but ...
MOLLY: But what if the 81 degrees lasts for many days, not just one?
ARTURO CASADEVALL: A heat challenge.
MOLLY: In that case, most of the fungus would die. But the more 81-degree days there are, the greater the chances that in the Russian roulette of evolution, one day you would get a fungus who's like, "You know what? I think I feel pretty okay." And the reason that fungus probably feels that way is because it has, like, a mutation of some sort.
ARTURO CASADEVALL: That gives it the capacity to survive the heat.
MOLLY: Maybe it can even fight a little harder.
ARTURO CASADEVALL: Turning on some of the defense mechanisms, like heat-shock proteins.
MOLLY: However it does it, this one fungus lives.
ARTURO CASADEVALL: And then it creates a copy of itself.
MOLLY: And then that fungus has fungus babies.
ARTURO CASADEVALL: What is called a bud.
MOLLY: And then that bud has buds.
ARTURO CASADEVALL: So the original cell may make 50 copies of itself before it basically runs out of fuel to make anymore, but those 50 ...
MOLLY: And so suddenly, you have a whole batch of fungus that survive at 81 degrees.
ARTURO CASADEVALL: Yeah.
JAD: Okay.
ARTURO CASADEVALL: And then after that, you take the survivors and you expose them to 90 degrees.
MOLLY: Let them sweat it out, and then—boom!—you got a whole batch at 90 degrees.
ARTURO CASADEVALL: You got it.
MOLLY: And you can just keep bumping this up degree by degree.
ARTURO CASADEVALL: Exactly.
MOLLY: A string of 91 degree days. 92 degree days, 93 degree days, 94 degree days.
ARTURO CASADEVALL: 95 degrees.
MOLLY: 96 degrees. 97 degrees. 98 degrees. And ultimately, 98.6 degrees.
ARTURO CASADEVALL: Now you have the capacity to survive inside the body of a human.
MOLLY: It reminds me of water. Like, if you're water and you go from 34° to 33°, you're still water, and 33° to 32°, you're still water. But there's this seemingly insignificant threshold between 32° to 31° that when you cross it, you become ice. And it is this almost minute transition that Arturo thinks happened with candida auris.
ARTURO CASADEVALL: That it was out there living in the environment, and it gradually adapted to be able to grow at a higher temperature. And when it did that, it acquired the capacity then to cause disease in people. Essentially, its adaptation defeated our heat defenses.
JAD: Wow!
MOLLY: Yeah. Yeah.
JAD: So fungus are being trained by the rising temperatures, and they're adapting along with those rising temperatures?
ARTURO CASADEVALL: You got it.
MOLLY: And then suddenly, it's not that far from, like, you know, that fungus in a soil getting caught on somebody's shoe, who walks it into a town that then goes into a hospital.
ARTURO CASADEVALL: Into an IV line. It can get into a wound, and then it can colonize patients.
JAD: Huh! That would explain why candida happened in all those places simultaneously. It was always in those places being tracked in on boots into hospitals, but only now it gets tracked in with this new ability to live in us.
MOLLY: Yes.
JAD: Wow!
[NEWS CLIP: Japan is suffering its hottest day on record.]
MOLLY: And this is an interesting thing. Like, all of a sudden, it made me think about all the headlines you see around the world.
[NEWS CLIP: Even in India, it's rarely been this hot.]
MOLLY: About, like ...
[NEWS CLIP: The country has been experiencing a deadly heat wave with dry air far hotter than the human body.]
MOLLY: "It's the 10th straight day above 105 degrees in Delhi."
[NEWS CLIP: All across the west.]
MOLLY: You know, or it's like ...
[NEWS CLIP: It was another day of oppressive heat.]
MOLLY: "Idaho's having the hottest August on record."
[NEWS CLIP: Funerals were underway in Karachi on Friday for some of the victims of the scorching heat wave.]
ARTURO CASADEVALL: You know, many people say when you tell them about this, "But how can that be? You know, they say that the average warmth, it may be one degree centigrade."
[NEWS CLIP: This is a so-called cooling station in Las Vegas.]
ARTURO CASADEVALL: I say that's not the right way to think about it. The right way to think about it is to imagine ...
[NEWS CLIP: Triple digit temperatures.]
ARTURO CASADEVALL: ... the number of really hot days, because each hot day is a hoop you gotta jump through.
MOLLY: And then just one last dash of interesting in looking at all this, like, fungus-temperature stuff: just as the fungus are learning to jump through our hoops, it turns out we are actually making it easier for them.
JAD: What do you mean?
MOLLY: So there was this paper recently that was talking about how the human body temperature has been declining. It's been steadily declining for decades at a rate of like 0.05 degrees Fahrenheit per decade.
JAD: Really?
MOLLY: Yeah.
JAD: So we're not 98.6 anymore. What are we?
MOLLY: They think it's actually more around, like, 97.5. But in fact ...
JAD: Interesting.
MOLLY: Do you get that a lot when you measure your kids?
JAD: Yeah, I'm always like, "Oh, you're not—you're colder."
MOLLY: The one thing that the researchers were talking about, though, in the declining, is that they looked at Western records, but, you know, they say—well, they did a small study on people in Pakistan, and they were more around 98.6. And the researchers were talking about how—essentially, how hard your body has to work to stay healthy. And consequently, the healthcare system that you're in is what is, like, affecting the temperature decline. So I don't think they think it's, like, worldwide. I think it's like a developed country, Western kind of thing.
JAD: I see. So in countries where there's more advanced healthcare, you're gonna see internal body temps start to lower.
MOLLY: Basically, yeah.
JAD: Whoa.
MOLLY: So essentially, in sum, there is, you know, this head to head between fungus and us. And it is a very fine line going from being insignificant to, you know, king or queen of the castle.
ARTURO CASADEVALL: Many organisms that you recover from the environment can only grow at environmental temperatures, but some of them have—it's a whole range of temperature susceptibilities or temperature resistance. That's an easy way to put it. And some of them happen to—their maximum happens to be just below your temperatures. And these are the ones that we worry about because many of them may have the capacity to cause disease, but they cannot do it because they cannot survive the higher temperatures.
MOLLY: Wait, what are the other ones that are just below my 98.6°?
ARTURO CASADEVALL: Well, there are probably—I don't want to be alarmist, but there are probably in the hundreds of thousands or even in the millions.
MOLLY: [laughs] I mean, I don't want to be alarmist either, but now I want to know what's, like, marching at my heels. Yeah.
ARTURO CASADEVALL: Right.
MOLLY: Wow, that's just so weird. Like, out of all the things that climate change can do to me, I was not thinking about, like, it's warming up microbes on the sidewalk and they're like, "Ah, finally! I can crawl into a human. This is the moment we've been waiting for for millions of years."
ARTURO CASADEVALL: It's some image. Yeah. [laughs]
MOLLY: Yeah.
JAD: Wow! Molly, thank you? I guess, for just giving me one more thing to have nightmares about.
MOLLY: Sure. I am always happy to seed your fears.
JAD: [laughs] This story was, of course, reported by Molly Webster, produced by Molly with Bethel Habte. Production help from Tad Davis. Special thanks to Luis Ostrowski. Until next time, I'm Jad Abumarad. Thanks for listening.
[LISTENER: Hi, this is Katie from Boulder, Colorado. Radiolab is created by Jad Abumrad with Robert Krulwich, and produced by Soren Wheeler. Dylan Keefe is our director of sound design. Suzie Lechtenberg is our executive producer. Our staff include Simon Adler, Jeremy Bloom, Becca Bressler, Rachael Cusick, David Gebel, Bethel Habte, Tracie Hunte, Matt Kielty, Tobin Low, Annie McEwen, Latif Nasser, Sarah Qari, Arianne Wack, Pat Walters and Molly Webster, with help from Shima Oliaee, Sarah Sandbach and Russell Gragg. Our fact checker is Michelle Harris.]
-30-
Copyright © 2024 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of programming is the audio record.